1. Introduction
Given the rapid aging of the Japanese population, both the number of patients with cancer and the percentage of cancer-related mortality among all deaths have been rising in this country. At present, one of every two individuals develops cancer and one out of three dies of cancer. The incidence of and deaths due to cancer are anticipated to continue rising in the foreseeable future. Radiotherapy is applicable to patients with cancer regardless of the type and condition of the malignancy. For this reason, in foreign countries, radiotherapy has been applied to more than half of all patients with cancer. In Japan as well, it is estimated that one out of four individuals will receive at least one form of radiotherapy in the future. The significance of radiotherapy has recently been recognized again as not only a palliative therapeutic approach but also as a means of radical treatment, and the demand for radiotherapy is expected to further increase henceforth. In April 2007, the Cancer Control Act came into effect in Japan. Providing better radiotherapy is one of the key goals of this law. Pursuant to the provisions of the law, the existing standards on facilities and equipment used for radiotherapy at core cancer care hospitals are being extensively reviewed. Radiotherapy equipment and adequate staff specializing in radiotherapy will become essential at such hospitals from 2010 onward, under the revised standards (Table 1). Also in the revision of the health insurance payment system (listing reimbursement amounts for healthcare services under the Japanese national health insurance scheme) in 2008, the payment amounts related to radiotherapy were substantially modified, evidently reflecting higher appraisal of the value of radiotherapy in healthcare policies of the government.
Herein, the author reviews progress in radiotherapy based on his 20-year career as a physician specializing in this field and provides future perspectives related to the devices and equipment used for radiotherapy.
| Table 1. Draft standard on facilities and equipment for core cancer care hospitals in 2010 (radiotherapy-related standards) |
(1) At least one full-time radiation oncologist
(2) At least one full-time radiological technologist specializing in radiotherapy
(3) At least one full-time quality manager specializing in radiotherapy
(4) Radiotherapy devices
|
2. Changes in radiotherapy
(1) 1988 (when the author joined the department of radiology) - 1994
The author joined the Department of Radiology, Chiba University School of Medicine, in 1988. In those days, radiotherapy played quite a small role as compared to surgical treatment, and most patients receiving radiotherapy had advanced or terminal stage cancer. The absolute number of patients receiving radiotherapy was very small. We radiologists seldom had a chance to apply radiotherapy as a means of radical treatment even for early cancer. Most of the patients admitted to radiology department ward had malignant lymphoma (the only disease for which radiotherapy had a competitive edge against surgical treatment). Even for these malignant lymphoma patients admitted to the department of radiology, chemotherapy was the major treatment, and radiotherapy served only as an adjuvant approach. I do not remember clearly why I selected this poorly highlighted field of radiotherapy. I may well have been inspired by a concern with palliative therapy. In addition, I recall the members of the department of radiology in those days being rather high-spirited.
At that time, there was no systematic education system for residency which could be called a “post-graduate initial training system.” I spent the early years of my career under unrestricted circumstances quite conducive to intellectual and academic freedom. About 3 years after entering this department, I found myself capable of making most judgments regarding radiotherapy independently. The positioning of radiotherapy to cancer treatment in those days was quite low as before, through my experiences of esophageal or head/neck cancer, which had already been abandoned by a surgeon, however, I could see that occasionally resolved completely by means of radiotherapy. And I had been getting a strong feeling that a cure should be more certain if radiotherapy could be applied at earlier stages.
Under these circumstances, Dr. Makoto Kondo, a physician at Keio University, gave several presentations (with titles such as “Patients, you should not fight cancer!”) or made statements sharply delineating the limitations or contradictions of surgical treatment at professional meetings, to the media, etc. in the first half of the 1990s. I believe that radiotherapy in Japan came into the spotlight during those years.
(2) 1994 – 2002 : Early attention to radiotherapy
In the 5th year after graduation, I was appointed to be a member of the Health Insurance Committee of the Japanese Society for Therapeutic Radiology and Oncology (JASTRO). As a member of that committee, I began to learn how the health insurance remuneration points for treatment system functions, particularly for radiotherapy. This system had been established within the framework of governmental healthcare policy, with the goal of being committed to reforming the decision-making process. The first task assigned to me as a member of the Health Insurance Committee was to prepare a dataset which would be useful for new setting insurer reimbursements of radiotherapy-related manipulations/services depending on the degree of difficulty/ease of individual manipulations/services. To this end, I conducted a questionnaire survey involving medical facilities nationwide. In response to the dataset presented by JASTRO, the government (insurer) revised the payment system of radiotherapy planning into a three-stage system reflecting the individual degree of difficulty/ease of it in 1996. This was a long-expected good news to all radiotherapy professionals. Four years later, in 2000, the payment system for radiotherapy technique was also changed into a three-stage system reflecting the degree of difficulty/ease, accompanied by adoption of new categories of payment for hyperfractionated irradiation and extra payment for radiology specialists. The number of patients managed at radiotherapy departments was steadily rising in those days, resulting in a sharp increase in the number of hospitals in which the radiology department was able to operate in the black, instead of the previous “red-ink section”1) (Table 2).
| Table 2. Annual changes in reimbursement for radiotherapy under national health insurance system in Japan |
Category |
|
1986 |
1992 |
1994 |
1996 |
2002 |
2004 |
2006 |
M000
|
Radiotherapy management
fee
|
1,000
|
2,000
|
2,500
|
|
|
|
|
| 1 |
Simple |
- |
- |
- |
2,600 |
2,700 |
2,700 |
2,700 |
| 2 |
Complex |
- |
- |
- |
3,000 |
3,100 |
3,100 |
3,100 |
| 3 |
Special |
- |
- |
- |
3,300 |
3,400 |
3,400 |
3,400 |
| |
Extra fee for
specialist in
radiotherapy
(for facilities
satisfying
certain
requirements) |
|
|
|
|
330 |
330 |
330 |
M001
|
Extracorporeal
irradiation
|
|
|
|
|
|
|
|
| 2 |
Massive
distant
cobalt-60
irradiation |
210 |
550 |
700 |
700 |
700 |
700 |
700 |
| 3 |
High-energy
radiotherapy |
320 |
800 |
950 |
1,000 |
|
|
|
| |
Simple |
|
|
|
|
930 |
930 |
930 |
| |
Complex |
|
|
|
|
1240 |
1240 |
1240 |
| |
Special |
|
|
|
|
1580 |
1580 |
1580 |
M001-2 |
Stereotactic radiotherapy with gamma-knife |
- |
- |
- |
70,000 |
63,000 |
63,000 |
50,000 |
M001-3 |
Stereotactic radiotherapy with linear accelerator |
- |
- |
- |
- |
- |
63,000 |
63,000 |
M004 |
Intracavitary prostate cancer irradiation |
|
|
|
|
|
|
48,600 |
|
(3) 2002 - : Mini-bubble-like prosperity
After 2002, I was given a chance to collect data on stereotactic radiotherapy for lung cancer from multiple facilities across the nation. Analysis of the collected data eventually revealed the outcomes of radiotherapy to not be inferior to those of surgical treatment. Publication of these results attracted media attention. We were interviewed by many journalists, and our treatment approach was reported with the catch phrase “Radiotherapy cures cancer without resection.” Furthermore, the radiation on certification system, established by JASTRO, was highly appraised by society, and employment of JASTRO-certified radiation oncologist was adopted as an indispensable element or requirement for third party appraisal of hospitals and even for accreditation of other medical departments.
In the early current decade, on the other hand, adverse accidents and errors in patient management related to radiotherapy were discovered at many facilities. These events were sensationally broadcast by the NHK TV Program “Today’s Close Up”, etc. These programs, however, were not based on a negative view of radiotherapy but rather focused on the inadequate infrastructure for radiotherapy, pointing out the necessity of quality management and the shortage of expert staff involved in radiotherapy, from a somewhat positive standpoint. Despite repeated media reports on adverse events associated with radiotherapy, the number of patients receiving radiotherapy continued to increase. As measures to promote an increase in the number of radiotherapy professionals, the Ministry of Health, Labour and Welfare (MHLW) adopted the uniform cancer management policy (aimed at minimizing differences in quality and level of cancer management among different districts or facilities) in 2005 and promulgated the Cancer Control Act in 2007. In response to these measures, medical facilities providing radiotherapy hastily introduced high-tech radiotherapy devices (Fig. 1). Mass media reported these trends in a manner lacking due insight, attaching primary importance to entertaining their readers. Therefore at present, the mini-bubble-like prosperity of radiotherapy, triggered more by imagination than firm contents, is seen in many places. In the presence of a common understanding that healthcare is not profitable at present, under the government’s stance of reducing national healthcare expenditures, close attention has been paid to the seemingly “profitable” and “attractive” radiotherapy, and a number of ill-trained or even untrained people with virtually no understanding of radiotherapy (irradiation device importers/dealers, hospital owners, investment companies and others) are now entering in this field. Considering the fragile infrastructure and environment related to radiotherapy in Japan, these bubbles should be recognized as thin-walled and likely to burst at any time 1-3).
 |

3. High-tech radiotherapy technology
Table 3 summarizes recent topics pertaining to radiotherapy. Radiotherapy technology has been undergoing rapid changes following recent advances in information technology. A particularly striking change in routine clinical practice during the past several years is the extensive adoption of devices for three-dimensional treatment planning. Among new techniques for radiotherapy planning, image fusion technology (super-imposing MRI or PET images on CT images), four-dimensional treatment planning (to deal with respiration-caused motions) and breath-holding techniques have begun to be adopted. So far as health insurance is concerned, stereotactic radiotherapy for the body was covered by insurance in 2004, and Intensity Modulated Radiation Therapy (IMRT) was also covered in 2008. Extensive adoption of these new techniques and further technological advances in radiotherapy are expected henceforth.

| Table 3. Recent radiotherapy topics |
- Image-guided radiotherapy (IGRT): Improved reproducibility, irradiation under CT guidance, image fusion (precise CTV and CTV enclosure)
- Reduction of respiration-caused motions:Respiration-gated irradiation, irradiation with breath-holding, dynamic chasing irradiation
- Target-specific irradiated field (multi-leaf three-dimensional conformation radiotherapy)
- Adaptive Radiotherapy (ART):Dealing with changes in the target during irradiation
- Advances in special forms of radiotherapy
Stereotactic radiotherapy (SRT)
Intensity-modulated radiotherapy (IMRT)
Small source radiotherapy (use of 131-I seed permitted)
Heavy particle radiation therapy
|
4. Why is the outcome of radiotherapy comparable to that of surgical treatment
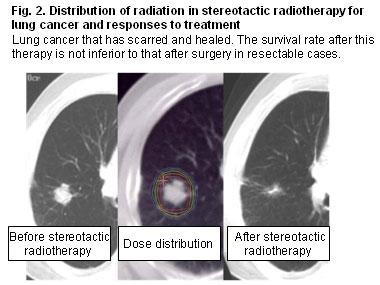
Fig. 2 shows a stage I lung cancer case who received the recently highlighted stereotactic radiotherapy (SRT) and Table 4 shows five-year survival rate of surgery and SRT for stage I lung cancer. The outcomes of radiotherapy for stage I lung cancer are presently approaching those of surgical treatment [4-8]. How stereotactic radiotherapy (pin-point irradiation to tumor-affected area alone) can yield outcomes comparable or superior to those of surgical treatment (resection of the tumor together with surrounding tissues and regional lymph nodes) may be explained as follows. One reason is that stereotactic radiotherapy causes no operative stress. Operative stress is known to induce massive release of cytokines and catecholamines. Cytokines stimulate tumor cell proliferation and metastasis, while catecholamines suppress cell-mediated immunity. Another reason is that unfavorable immune power reduction of tumor cell trapping and antigen-antibody reactions due to regional lymph node excision was produced after surgery but was minimized by stereotactic radiotherapy because they can be avoided. Radiotherapy is now attracting close attention as a substitute for surgery. This is because the results of body-friendly radiotherapy, which does not involve operative stress or regional lymph node excision, have been clinically shown to be potentially comparable or superior to those of surgery. This feature of stereotactic radiotherapy should also be applicable to three-dimensional radiotherapy which employs IMRT or other advanced irradiation techniques. The roles played by these high-accuracy radiotherapy techniques are anticipated to expand henceforth.
 |
| Table 4. Outcomes compared with standard surgery (uncorrected 5-year survival rate) |
| Stage |
USA 6) |
NationalCancerCenter 7) |
Nationwide average 8) |
Stereotactic radiotherapy 4) |
|
| T1N0M0 |
61% |
71% |
72% |
77% |
| T2N0M0 |
40% |
44% |
50% |
68% |
|
|

5. Radiotherapy in the future
(1) The future for number of patients receiving radiotherapy (Fig. 3)
The number of patients receiving radiotherapy has been steadily increasing. It has doubled during the past decade, reaching nearly 160,000 in 2005. There will be another two-fold increase in the coming decade 2,3). It is highly probable that the increase in this number is accelerated by the factors listed in Table 5. From 2030 onward, the number of patients receiving radiotherapy may stop increasing and plateau due to a decrease in the entire population and changes in the population age distribution .
| Table 5. Factors increasing the demand for radiotherapy in the future |
- Increase in cancer patients and necessity for less invasive treatment in aging societies
- Spread of evidence-based medicine and self-selection of treatment methods
- Therapeutic strategy emphasizing quality of life
- Medico-economic evaluation of radiotherapy
- Priority given to radiotherapy under healthcare policy (based on Cancer Control Act )
- Further advances in irradiation technology
|
(2) Predictions as to radiotherapy devices needed in the future: estimated annual demand for 100 new linear accelerators
Because the standards for facilities and equipments for core cancer care hospitals were amended, as stated above, radiotherapy devices satisfying the new standards will be installed immediately at 19 such hospitals. Assuming that the number of patients receiving radiotherapy 10 years later is 400,000 (240,000 more than at present), 1,333 linear accelerators will be needed at that time, if each device is used for 300 patients annually as suggested in the Japanese Blue Book (published by the Teshima Group under the MHLW-subsidized cancer research program) 9). Because the total number of linear accelerators available as of 2003 was 750, an additional 583 devices need to be installed (58 devices/year) to meet this demand. If existing devices are renewed at a pace of 40/year, approximately 100 new devices would need to be installed annually during the coming decade. Simple calculations regarding the demands for other devices needed for radiotherapy are difficult because they depend on the number of facilities providing radiotherapy and the efficiency of staff members allocated to individual facilities. However, taking into account the estimated increase in the number of patients receiving radiotherapy and the need for more complex and sophisticated treatment planning, it is plausible that a greater number of auxiliary devices and more frequent renewal of these devices will be necessary.

6. Problems with the rise and spread of radiation-related devices
At a glance, it appears that radiotherapy department profits can be easily increased if the payment amounts for radiotherapy-related manipulations/services under the national health insurance system are modified upwards. In practice, however, radiotherapy departments require investment in land and buildings in addition to facilities and equipment. Furthermore, radiation devices must be renewed in 10-year or shorter cycles. Moreover, in Japan, the number of patients and the number devices at radiology departments are in a precarious balance with the number of personnel working in the radiotherapy field. In Japan, the professions involved in radiotherapy are not diverse and are limited to a few categories. As a result, physicians specializing in radiotherapy are often forced to also be involved in quality control of radiotherapy and clerical work related to the therapy due to the lack of adequate staff specifically assigned to these duties 2,3). We can find that many of the adverse patient incidents related to radiotherapy, which came to light in the 2002 through 2004 period, were at least partially attributable to fatigue, i.e. overworked physicians and technologists, and the absence of staff specializing in quality control. Following enactment of the Cancer Control Act which refers to the necessity of strengthening the infrastructure for radiotherapy, payment under the health insurance system for quality control of radiotherapy was adopted as a “fee for safety and equipment management” when the health insurance payment system was revised in 2008. However, when viewed on a national scale, the infrastructure for radiotherapy in Japan is still quite fragile in terms of both staff and system operation. At present, the most important aspect of meeting the estimated increase in the demand for radiotherapy-related devices, is system improvement to ensure safe radiotherapy. To this end, it will be necessary to develop an adequate number of quality control managers in charge of safety management as well as medical engineers (who support physicians in treatment planning) and nursing staff and others specializing in clerical work, etc. associated with radiotherapy. These measures must be accompanied by an urgent effort to increase the absolute number of physicians specializing in radiotherapy. The government, professional societies (JASTRO) and universities should cooperate in reaching this difficult goal. To put it concretely, it is important to facilitate incorporation of an independent course in radiation oncology at medical schools and to improve the education and training of medical students and residents. Furthermore, for efficient allocation of facilities, devices and physicians specializing in radiotherapy, it is essential to reorganize medical facilities involved in radiotherapy, i.e., to integrate radiotherapy within regional core or higher-level hospitals (central facilities) under improved linkage with satellite facilities.

7. Development of radiotherapy technology needs to be accompanied by development of diagnostic imaging technology
Table 6 lists new irradiation techniques and the development of which is expected (or desirable). Needless to say, advances in radiotherapy technology are closely linked to the development and application of imaging technology. In Japan, there is a growing tendency for courses in diagnostic imaging and radiation oncology to be organized as independent units at medical schools. In any event, it will be essential that all physicians, technologists and manufacturers exchange information with each other as to the needs and technology related to diagnostic imaging and radiotherapy.
| Table 6. Anticipated future developments in radiotherapy techniques |
- Compact and high-voltage acceleration tube
- Irradiation devices with large rotation diameter (clearance)
- Identification of tumor location and shape by diagnostic imaging
- Automated correction of set-up error
- Improved accuracy in controlling respiration-caused motions
- Application of molecular imaging
- Optimization of biological effect model and its application to treatment planning devices
|
8. At the end – It’s Ideal shape in the business field. (My wish)
Radiotherapy is now a symbol of high-tech healthcare. Many journalists visit radiology departments to collect information about this therapy. However, because media reports tend to lack adequate insight, readers often have erroneous images or unrealistic expectations about radiotherapy (e.g., “an almighty method of curing sickness, without adverse reactions”). Excessive attention and/or unrealistic expectations, slightly resembling the previous bubble economy, now seem to prevail in society, and many hospitals are extremely interested in introducing new radiotherapy devices and an rather excessive number of radiotherapy clinics have thus been established.
The author speculates that under such circumstances, the enterprises involved in radiation devices will receive an increasing number of inquiries or offers from clients. The author would like to take this opportunity to ask these enterprises to be cautious of marketing while maintaining adequate insight into the necessity of preserving appropriate and sound radiotherapy for the future. In other words, the author hopes that business interests will refrain from “selling as many products as possible”, instead selling their products only to those facilities capable of appropriately using the products (based on prior survey and assessment of individual clients). It seems advisable for enterprises to bear in mind that although irresponsible marketing may produce temporary profits, such a stance carries the risk of reducing reliance on radiotherapy and the hazards of bad debt in the long run, since the current prosperity in radiotherapy-related business looks like a bubble 2). To assure that radiotherapy can become a basic tool for cancer management, enhancing the daily lives of people, it seems essential that healthcare providers, enterprises and government agencies adopt careful, solid and strategic radiotherapy policies 3).

<Acknowledgments>
The author is indebted to Dr. T. Dokiya (Saitama Medical University), Dr. T. Teshima and Dr. H. Numasaki (Osaka University) and Mr. Y. Ashino (CMS Japan) for their cooperation and advice during data collection.
<References>
1) Onishi H. Contribution of radiotherapy to hospital management and problems involved – Special reference to health insurance payment system and efficacy in cancer treatment. Magazine of Medical Industry. 2007 Dec; 51-54.
2) Onishi H, Araki T, Yamashita T, Hiroakwa Y, Karasawa K, Uno T, Yorozu A, Takahashi Y and Ashino Y. Current status of radiotherapy staff and devices in Japan – Quality assurance and reduction of errors related to radiotherapy. Gan To Shukushu. 2004;16:191-199.
3) Onishi H, Araki T and Nakagawa K. Current status and countermeasures on shortage of personnels involved in radiotherapy. Monthly Journal of Medical Imaging and Information. 2005;37:1231-1235.
4) Onishi H, Shirato H, Nagata Y, et al. Hypofractionated stereotactic radiotherapy (HypoFXSRT) for stage I non-small cell lung cancer: updated results of 257 patients in a Japanese multi-institutional study. J Thorac Oncol. 2007 Jul;2(7 Suppl 3):S94-100.
5) Onishi J, Sano N and Araki T. Stereotactic radiotherapy for the trunk – Current status and future of its innovative significance. Japanese Journal of Clinical Radiology. 2006;51:583-595.
6) Mountain CF. Semin Surg Oncol 18:106-115,2000.
7) Shirakusa T, Kobayashi K. Lung Cancer in Japan: analysis of lung cancer registry for resected cases in 1994. Japanese Journal of Lung Cancer 42:555-562,2002.
8) Naruke T,Tsuchiua R, Kondo H, et al. Ann Thorac Surg 71:1759-1764,2001.
9) Teshima Group under the MHLW-Subsidized Cancer Research Program (14-6). Radiology and oncology in multi-disciplinary treatment of cancers – Infrastructure needed to ensure the quality of radiotherapy based on the findings from a field survey. |

